Table of Contents
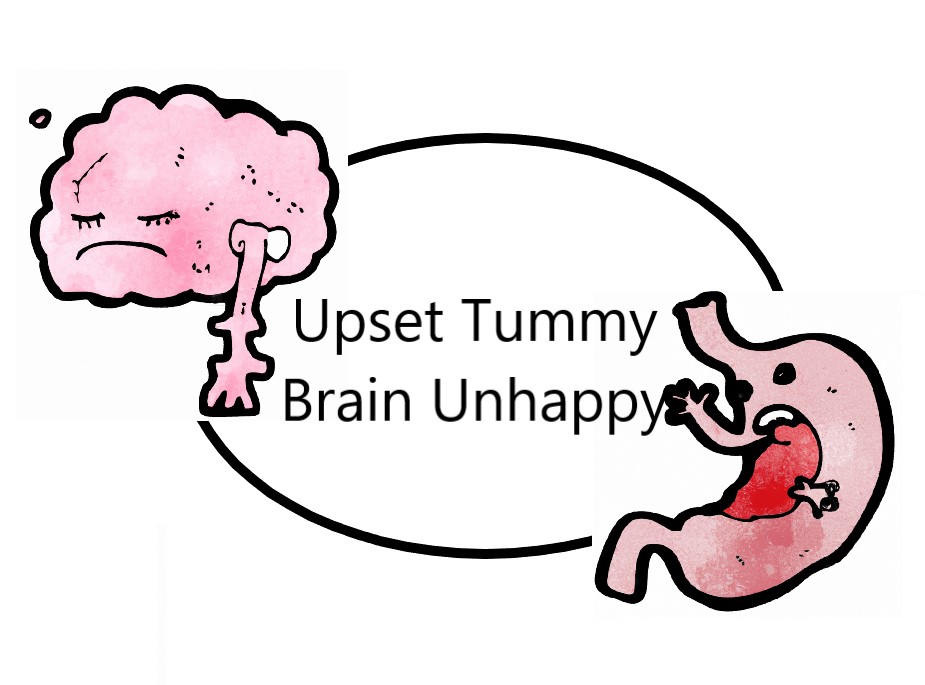
Gut and Brain
The gut-brain connection is a complex network of interactions between the central nervous system (CNS) and the enteric nervous system (ENS). This connection allows bidirectional communication between the gut and the brain through the nervous system, immune system and endocrine system. One of the main pathways involved in the gut-brain axis is the vagus nerve, which connects the ENS to the CNS. The vagus nerve is the largest nerve of the parasympathetic nervous system, which is responsible for rest and digest functions. The vagus nerve sends signals from the gut to the brain, and from the brain to the gut, which can affect gut motility, gut secretion, and gut immune function. The vagus nerve also plays a role in regulating the release of neurotransmitters, such as acetylcholine and norepinephrine, which can affect brain function.
Research has shown that a healthy gut microbiome is crucial for maintaining optimal mental health and that imbalances in gut bacteria can contribute to the development of mental health disorders such as anxiety and depression. The gut-brain axis has been implicated in a wide range of neurological and psychiatric disorders, including Parkinson’s disease, Alzheimer’s disease, depression, and anxiety. Dysfunction of the gut-brain axis has been suggested to contribute to the pathogenesis of these disorders.
Studies have also shown that people with mental health disorders such as depression and anxiety tend to have different gut microbiota profiles compared to healthy individuals. For example, one study found that people with depression had reduced levels of certain bacteria in their gut, including Faecalibacterium and Coprococcus, which are known to produce anti-inflammatory compounds.
Some Functions of Gut Microbiota/Bacteria:
- Produce short-chain fatty acids (SCFAs), which are important for maintaining the integrity of the gut lining and regulating immune function. Studies have found that individuals with mood disorders such as depression have lower levels of SCFAs, indicating an imbalance in gut bacteria.
- Produce neurotransmitters such as cortisol (stress hormone), serotonin, dopamine, and gamma-aminobutyric acid (GABA), which are essential for regulating mood, anxiety, and stress. Stress, especially chronic stress, can lead to an imbalance in gut bacteria, which can, in turn, lead to the development of mental health disorders. When the body is under stress, the sympathetic nervous system is activated, which can lead to changes in gut motility, permeability, and the composition of the gut microbiota.
- Regulates the immune system. An imbalance in gut bacteria, such as from antibiotic use, a high-fat diet, or stress, can lead to changes in neurotransmitter production and activity, as well as inflammation in the gut and brain. Inflammation is a normal response of the immune system to injury or infection, but chronic inflammation has been linked to a range of mental health disorders, including depression, anxiety, and schizophrenia.
- Supports gut’s permeability. Gut permeability refers to the degree to which the gut allows substances to pass through its walls into the bloodstream. When the gut is healthy, it only allows necessary nutrients to pass through, but when it is damaged, it can allow harmful substances such as bacteria and toxins to enter (Gut leak) the bloodstream, leading to inflammation and potential harm to the brain (neurodegeneration).
Link to Parkinson’s Disease
In recent years, there has been growing interest in the link between the gut microbiome and neurological disorders such as Parkinson’s disease. One study found that people with Parkinson’s disease have a different gut microbiome composition than healthy individuals. Specifically, they had lower levels of bacteria that produce short-chain fatty acids (SCFAs). Another study found that a particular strain of bacteria, called Akkermansia muciniphila, was significantly reduced in people with Parkinson’s disease compared to healthy individuals. This strain of bacteria has been shown to have anti-inflammatory properties and to improve gut barrier function. In addition, studies have found that individuals with Parkinson’s disease have increased intestinal permeability.
Research has also shown that the gut microbiome may be involved in the development and progression of Parkinson’s disease. In animal studies, researchers have found that disrupting the gut microbiome can lead to an increase in alpha-synuclein protein, which is a hallmark of Parkinson’s disease. This suggests that the gut microbiome may play a role in the aggregation of alpha-synuclein and the formation of Lewy bodies, which are a key feature of Parkinson’s disease.
A recent review of studies on the gut microbiome in Parkinson’s disease concluded that there is evidence to support the role of gut dysbiosis (disruption to Microbiome) in the pathogenesis of Parkinson’s disease. The review also found that certain dietary interventions and probiotics can modulate the gut microbiome and improve symptoms in individuals with Parkinson’s disease.
Ways to Improve Health thru Gut
It is clear by now that maintaining a healthy gut microbiome is important for everyone, especially for people with Parkinson’s disease. Here are several ways to protect and improve gut health:
Eat a healthy, balanced diet
(See also Natural Ways To Avoid Constipation)
A diet that is high in fiber, fruits, vegetables, lean protein sources, and whole grains can help promote the growth of beneficial gut bacteria and improve gut health. A dietary intervention that has shown promise is the Mediterranean diet, which is rich in fruits, vegetables, whole grains, and healthy fats. A study found that adherence to the Mediterranean diet was associated with a reduced risk of Parkinson’s disease.
- Fiber: Soluble and insoluble fibers provide bulk to the stool, promote regular bowel movements, and serve as a prebiotic to feed beneficial gut bacteria. The recommended daily intake of fiber varies depending on age, gender, and physical activity level. Generally, the recommended daily intake of fiber is:
- For adult women: 25 grams per day
- For adult men: 38 grams per day
However, some experts suggest that people should aim for even higher amounts of fiber, such as 30-40 grams per day, to further promote gut health and reduce the risk of chronic diseases. While fiber is important for gut health, consuming too much fiber can have side effects on the gut.
- Bloating and gas: Consuming too much fiber can cause bloating and gas, especially if you increase your fiber intake too quickly.
- Constipation or diarrhea: Consuming too much fiber can cause constipation or diarrhea, depending on the type of fiber and how much water you drink.
- Nutrient deficiencies: Consuming too much fiber can interfere with the absorption of certain nutrients, such as iron, calcium, and zinc.
- Intestinal discomfort: Consuming too much fiber can cause intestinal discomfort, such as cramping and abdominal pain.
It is important to note that the amount of fiber that is considered “too much” can vary from person to person and depends on factors such as age, gender, and physical activity level.
- Probiotic: Probiotics are live microorganisms that provide health benefits to the host by restoring and maintaining the balance of gut bacteria. Look for a probiotic supplement that contains a variety of strains of bacteria. One study found that probiotics can improve symptoms of depression and anxiety in people with irritable bowel syndrome (IBS). Probiotics, when consumed, have also been studied for their potential therapeutic benefits in Parkinson’s disease. On another study the use of a specific strain of probiotic led to improvements in motor function and reduced inflammation in individuals with Parkinson’s disease.
- Prebiotics: Non-digestible fibers that serve as food for beneficial gut bacteria. A study found that the use of prebiotics led to improvements in motor function and reduced inflammation in individuals with Parkinson’s disease.
- Fermented foods: Fermented foods, such as yogurt, kefir, and kimchi, are rich in beneficial bacteria that can help improve gut health.
- Polyphenols: Plant compounds that have anti-inflammatory and antioxidant properties, which can reduce inflammation in the gut.
- Omega-3 fatty acids: Essential fatty acids that have anti-inflammatory properties and can help reduce inflammation in the gut. Another study found that a dietary intervention that included probiotics, prebiotics, and omega-3 fatty acids improved depression and anxiety symptoms in people with major depressive disorder.
- Vitamin D: A nutrient that is important for gut health, as it regulates the immune system and can reduce inflammation in the gut.
- Zinc: An essential mineral that is important for maintaining a healthy gut lining and preventing leaky gut.
Stay hydrated
Drinking enough water can help promote regular bowel movements and prevent constipation, which is pretty common with PD patients.
Manage stress
Stress, especially chronic stress, can disrupt the gut microbiome and lead to inflammation. Engage in stress-reducing activities such as meditation, yoga, or deep breathing exercises.
Get enough sleep
Lack of sleep can disrupt the balance of gut bacteria and lead to inflammation in the gut.
Avoid antibiotics unless necessary
Antibiotics can disrupt the balance of gut bacteria, so it is important to avoid them unless they are necessary. Talk to your doctor about alternatives if possible.
In summary, the gut-brain connection is a complex and bidirectional relationship through the gut-brain axis, with disruptions in gut health potentially leading to changes in neurotransmitter production, inflammation, and harmful substances entering the bloodstream. Improving gut health through dietary changes, exercise, probiotics, and other various interventions may have positive effects on overall health, especially for Parkinson’s disease patients.
References:
- Anderson, J. W., Baird, P., Davis Jr, R. H., Ferreri, S., Knudtson, M., Koraym, A., … & Williams, C. L. (2009). Health benefits of dietary fiber. Nutrition reviews, 67(4), 188-205.
- Bedarf, J. R., Hildebrand, F., Coelho, L. P., Sunagawa, S., Bahram, M., Goeser, F., … & Bork, P. (2017). Functional implications of microbial and viral gut metagenome changes in early stage L-DOPA-naïve Parkinson’s disease patients. Genome medicine, 9(1), 39.
- Braak, H., & Del Tredici, K. (2018). Neuropathological staging of brain pathology in sporadic Parkinson’s disease: separating the wheat from the chaff. Journal of Parkinson’s disease, 8(s1), S71-S85.
- Calder, P. C. (2015). Marine omega-3 fatty acids and inflammatory processes: Effects, mechanisms and clinical relevance. Biochimica et Biophysica Acta (BBA)-Molecular and Cell Biology of Lipids, 1851(4), 469-484.
- Cassani, E., Barichella, M., Cancello, R., Cavanna, F., Iorio, L., Cereda, E., … & Pezzoli, G. (2019). Probiotics and prebiotic fiber for constipation associated with Parkinson disease: An RCT. Neurology, 93(24), e2224-e2232.
- Chumpitazi, B. P., & Shulman, R. J. (2018). Dietary fiber and the human gut microbiota: application of evidence mapping methodology. Nutrition Reviews, 76(8), 568-585.
- Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience, 13(10), 701-712.
- Dehghan, P., & Pourghassem Gargari, B. (2021). Effects of excessive intake of dietary fiber on gastrointestinal disorders: A systematic review and meta-analysis. Nutrition, 87, 111204.
- Dinan, T. G., & Cryan, J. F. (2017). The microbiome-gut-brain axis in health and disease. Gastroenterology clinics, 46(1), 77-89.
- Forsyth, C. B., Shannon, K. M., Kordower, J. H., Voigt, R. M., Shaikh, M., Jaglin, J. A., … & Farrugia, G. (2011). Increased intestinal permeability correlates with sigmoid mucosa alpha-synuclein staining and endotoxin exposure markers in early Parkinson’s disease. PloS one, 6(12), e28032.
- Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305-12.
- Gao, X., Chen, H., Fung, T. T., Logroscino, G., Schwarzschild, M. A., & Hu, F. B. (2007). Prospective study of dietary pattern and risk of Parkinson disease. The American journal of clinical nutrition, 86(5), 1486-1494.
- Gibson, P. R., & Rosella, O. (2015). Zinc in gastrointestinal and liver disease. Gut, 64(8), 1390-1399.
- Hansen, I. S., & Krych, L. (2021). Gut Microbiota in Parkinson’s Disease: A Bourgeoning Role in Pathogenesis and Therapeutics. Movement Disorders, 36(3), 451-461.
- Hill, C., Guarner, F., Reid, G., Gibson, G. R., Merenstein, D. J., Pot, B., … & Salminen, S. (2014). Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature reviews Gastroenterology & hepatology, 11(8), 506-514.
- Hill-Burns, E. M., Debelius, J. W., Morton, J. T., Wissemann, W. T., Lewis, M. R., Wallen, Z. D., … & Knight, R. (2017). Parkinson’s disease and Parkinson’s disease medications have distinct signatures of the gut microbiome. Movement disorders, 32(5), 739-749.
- Hsiao, E. Y., McBride, S. W., Hsien, S., Sharon, G., Hyde, E. R., McCue, T., … & Mazmanian, S. K. (2013). Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell, 155(7), 1451-1463.
- Institute of Medicine (US) Panel on the Definition of Dietary Fiber; Woteki, C. E.; Tershakovec, A. M.; et al., editors. (2001). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academies Press (US).
- Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
- Marco, M. L., Heeney, D., Binda, S., Cifelli, C. J., Cotter, P. D., Foligné, B., … & Smid, E. J. (2021). Health benefits of fermented foods: microbiota and beyond. Current opinion in biotechnology, 70, 1-8.
- Mayer, E. A., Knight, R., Mazmanian, S. K., Cryan, J. F., & Tillisch, K. (2014). Gut microbes and the brain: paradigm shift in neuroscience. The Journal of neuroscience, 34(46), 15490-15496.
- Mayer, E. A., Tillisch, K., & Gupta, A. (2015). Gut/brain axis and the microbiota. Journal of clinical investigation, 125(3), 926-938.
- McRorie, J. W., & McKeown, N. M. (2017). Understanding the physics of functional fibers in the gastrointestinal tract: an evidence-based approach to resolving enduring misconceptions about insoluble and soluble fiber. Journal of the Academy of Nutrition and Dietetics, 117(2), 251-264.
- Monda, V., Villano, I., Messina, A., Valenzano, A., Esposito, T., Moscatelli, F., … & Precenzano, F. (2017). Exercise modifies the gut microbiota with positive health effects. Oxidative medicine and cellular longevity, 2017.
- Mulak, A., & Bonaz, B. (2015). Brain-gut-microbiota axis in Parkinson’s disease. World journal of gastroenterology, 21(37), 10609-10620.
- Petrov, V. A., Saltykova, I. V., Zhukova, I. A., Alifirova, V. M., Zhukova, N. G., Dorofeeva, Y. B., … & Tyakht, A. V. (2017). Analysis of gut microbiota in patients with Parkinson’s disease. Bulletin of experimental biology and medicine, 162(6), 734-737.
- Pinto-Sanchez MI, Hall GB, Ghajar K, Nardelli A, Bolino C, Lau JT, et al. Probiotic Bifidobacterium longum NCC3001 reduces depression scores and alters brain activity: a pilot study in patients with irritable bowel syndrome. Gastroenterology. 2017;153(2):448-459.e8.
- Rogers, G. B., Keating, D. J., Young, R. L., Wong, M. L., Licinio, J., & Wesselingh, S. (2016). From gut dysbiosis to altered brain function and mental illness: mechanisms and pathways. Molecular psychiatry, 21(6), 738-748.
- Sampson, T. R., & Mazmanian, S. K. (2015). Control of brain development, function, and behavior by the microbiome. Cell host & microbe, 17(5), 565-576.
- Scheperjans, F., & Eberhard, D. A. (2021). The role of the gut microbiome in Parkinson’s disease: a systematic review and meta-analysis. Gut Microbes, 13(1), 1-22.
- Scheperjans, F., Aho, V., Pereira, P. A., Koskinen, K., Paulin, L., Pekkonen, E., Haapaniemi, E., Kaakkola, S., Eerola-Rautio, J., Pohja, M., Kinnunen, E., Murros, K., Auvinen, P. (2015). Gut microbiota are related to Parkinson’s disease and clinical phenotype. Movement disorders, 30(3), 350-358.
- Selma, M. V., Tomás-Barberán, F. A., & Beltrán, D. (2019). Dietary polyphenols and gut microbiota: The bad guys or the good guys? Trends in Food Science & Technology, 75, 24-35.
- Singh, R. K., Chang, H. W., Yan, D., Lee, K. M., Ucmak, D., Wong, K., … & Liao, W. (2017). Influence of diet on the gut microbiome and implications for human health. Journal of translational medicine, 15(1), 73.
- Slavin, J. (2013). Fiber and prebiotics: mechanisms and health benefits. Nutrients, 5(4), 1417-1435.
- Smriga M, Ando T, Akutsu M. Oral treatment with L-lysine and L-arginine reduces anxiety and basal cortisol levels in healthy humans. Biomed Res. 2007;28(2):85-90.
- Tan, A. H., Lim, S. Y., Tan, Y. Y., Lee, S. C., Wang, Y. T., Ng, Y. S., … & Ng, S. C. (2019). Indigestible carbohydrate intake reduces the risk of Parkinson’s disease. Frontiers in aging neuroscience, 11, 333.
- Valles-Colomer, M., Falony, G., Darzi, Y., Tigchelaar, E. F., Wang, J., Tito, R. Y., … & Raes, J. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature microbiology, 4(4), 623-632.
- Wallace CJK, Milev R. The effects of probiotics on depressive symptoms in humans: a systematic review. Ann Gen Psychiatry. 2017;16(1):14.
- Wang, Y., & DeLuca, H. F. (2011). Is vitamin D deficiency a risk factor for osteoporosis? Proceedings of the National Academy of Sciences, 108(Supplement 2), 11776-11781.
- Zhang, Q., Hu, X. T., Chen, W., & Bao, C. J. (2021). Altered gut microbiome in Parkinson’s disease: A systematic review. Parkinsonism & related disorders, 83, 49-55.


















Leave a Reply